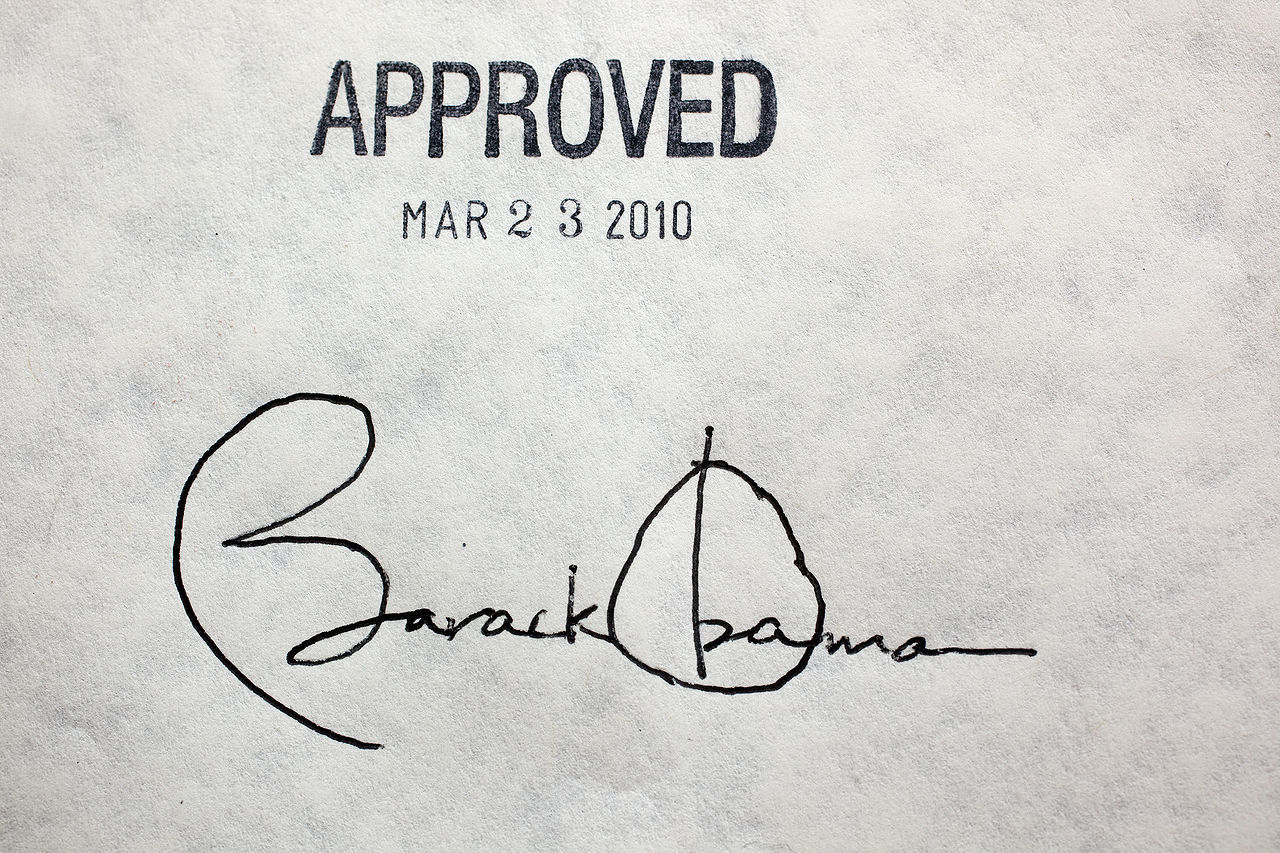
The Patient Protection and Affordable Care Act, commonly known as Obamacare, was signed into law on March 23, 2010. It represents the most significant regulatory overhaul of the U.S. healthcare system since the passage of Medicare and Medicaid in 1965. However, long-term effects of the shake-up are not self-contained within the healthcare industry. If Obamacare ultimately proves successful, it could serve as the model for regulatory overhaul for a variety of industries.
The Patient Protection and Affordable Care Act, commonly known as Obamacare, was signed into law on March 23, 2010. It represents the most significant regulatory overhaul of the U.S. healthcare system since the passage of Medicare and Medicaid in 1965. However, long-term effects of the shake-up are not self-contained within the healthcare industry. If Obamacare ultimately proves successful, it could serve as the model for regulatory overhaul for a variety of industries.
The intricacies of the Affordable Care Act are complex; however, in basic terms, it essentially lays out three broad mandates. First, no individual may be denied healthcare coverage because of a pre-existing condition. Second, if you do not work for a company that provides health insurance, you are required to purchase healthcare independently. If that is unaffordable at your income level, the government will subsidize. Finally, all health insurance plans are required to provide a certain minimum level of service.
In practice, these mandates create a difficult matrix for healthcare providers. They must provide health insurance to everyone, at a very high quality, within a highly regulated environment while operating as an economically viable entity (making a profit). Although challenging, this marriage of public sector regulation with private sector efficiencies promotes creative, unconventional, and ultimately successful results. For example, in the past, health insurance providers have garnered profit by keeping costs low because they focus on covering healthy individuals. While this system allowed insurance companies to make a profit, it inadvertently put a significant burden on hospital systems. When uninsured individuals would run up an unpayable medical bill, the hospital would be left eating the cost. From a high level view, this system put much of the risk insurance companies are designed to take on healthcare providers. It was economically viable but structurally inefficient.
Post Affordable Care Act, health insurance providers are required to provide coverage to everyone, so instead of discriminating among their customer base, they creatively squeeze profits from an entirely different angle. One example is new ‘narrow network’ plans where instead of leaving out people, they leave out hospitals, only covering a limited set of medical facilities. While seemingly counter-intuitive, these plans provide advantages to all parties. Insurance companies keep costs low by only covering a small set of hospitals and facilities. Hospitals are able to charge lower rates because they don’t eat costs from uninsured patients, and patients benefit because insurance providers can focus on premier care from a smaller group of facilities. Presuming the consumer remains conscious of where their insurance is accepted, narrow network plans are advantageous to everyone. This is just one example of how public sector regulation and private sector economic strategy can come together to form a system greater than the sum of its parts.
The marriage of public sector initiatives with private sector production is not new. Think wartime tank production in Ford car factories for quick mobilization or Georgia Power for long term infrastructure. Both examples represent government outsourcing for efficiency sake. What makes the healthcare overhaul unique is that the industry is equally as service based (doctors, nurses, patients) as infrastructure based (hospitals, pharmaceuticals, and biotech). This hybrid industry structure is naturally handled best by dexterous market forces. For example, nurses today have longer careers and perform more diverse tasks than ever before. As our population ages and demand increases for out of hospital nurses such as in the home or in secondary care facilities, nurses are able to extend their careers by taking on less physically demanding roles. Such examples of shifts to meet demographic demand are consistent across the industry and symptomatic of the healthcare industries ability to shift and evolve.
Potential implications of a successful industry reform are broad and extend beyond healthcare. For example, the higher education industry operates similarly to healthcare in many ways. It involves governmental oversight of an extensive network of largely independent organizations. Educational quality has come under fire in recent years. More and more people are demanding access to higher education, and finally, structural inefficiencies, such as overpopulated schools and overly complex bureaucracy, leave the industry ripe for reform. The idea of the government mandating public colleges to make their application process more transparent and their course offerings more consistent is not only possible but plausible. A successful Affordable Care Act could very well serve as the cultural touch point and model for expanding and improving publically regulated industries in a regulated, organized and efficient manner.